This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.

Building a climate-resilient healthcare system: The importance of adaptation & health infrastructure
OVERVIEW
The impact of climate change on our society and our healthcare system more specifically is no longer tomorrow’s problem, but one healthcare leaders are being forced to grapple right now, even in this time of unprecedented upheaval exacerbated by COVID-19.
Health and wellbeing and the effects of a changing climate are intricately linked. If governments are serious about action to fight the climate crisis, they must urgently invest in the infrastructure necessary to build a climate-resilient health system.
CLIMATE-RESILIENT HEALTH SYSTEMS
A climate-resilient health system anticipates, plans, responds, and recovers from climate-related stresses and protects and strengthens population health[i]. Building resilience means continuously adapting to the changing health risks caused by climate change that will affect the population and service delivery by a health system.
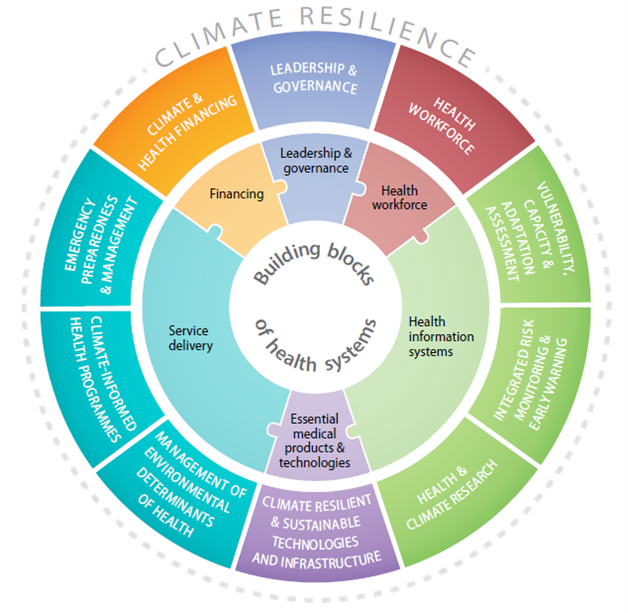
The World Health Organization (WHO) has developed an operational framework for building climate-resilient healthcare systems (Figure 1). The framework consists of 10 components that together provide an approach to integrating climate resilience into existing health systems[ii]. Health organizations, ministries of health, and other health agencies worldwide are using the WHO framework to assess and improve climate resiliency in health policies and programs[i].
Regional health authorities throughout Canada are also using the WHO framework to focus their adaptation efforts to transition to a sustainable and resilient health system. Health authorities need to prepare health facilities and clinical services to be able to respond to the impacts of climate change. Adaptation to climate change is essential, even with the most ambitious mitigation efforts to reduce greenhouse gas (GHG) emissions.
Figure 1: Ten components comprising the WHO operational framework for building climate-resilient health systems.
(Source: https://www.who.int/publications/i/item/9789241565073)
CANADA’S ADAPTATION STRATEGY
Actions to prepare populations and health systems for climate change, and reduce GHG emissions, can delay the increase in health risks from climate hazards.
Without ramping-up efforts at adapting to climate change impacts, health services will face increasing pressure. Adaptation measures such as assessments of risks and vulnerabilities can help transform health infrastructure and build climate resiliency. Conducting a vulnerability, capacity, and adaptation assessment is an important, proactive step in the process to create climate-resilient health systems. Two health authorities in British Columbia – Vancouver Coastal Health and Fraser Health – have together undertaken a vulnerability assessment of their respective health authorities (see Box 1).
Box 1: Vancouver Coastal Health and Fraser Health’s Climate Change and Health Vulnerability and Capacity Assessment
Vancouver Coastal Health (VCH) and Fraser Health partnered with Health Canada on a three-year funded grant to undertake a climate change and health vulnerability and adaptation assessment[iii]. The first phase assessed the degree to which population health, healthcare facilities, and certain health services are susceptible to, and prepared for, extreme heat, wildfires and air quality, severe storms, flooding, and more. The second phase of the project will involve the development of an adaptation framework for VCH and Fraser Health. The framework will present priorities and actions corresponding to the vulnerabilities identified in the assessment and define the role of the health authorities.
Many health authorities in Canada are increasing their adaptation efforts, tailored to their local context. However, adaptation must be rapidly scaled up to protect Canadians and our nation’s healthcare systems.
The Government of Canada is developing Canada’s National Adaptation Strategy, which is expected to be completed by December 2022. The adaptation strategy will be a shared vision for climate resilience across Canada and focuses on five priorities:
- Thriving natural environment;
- Disaster resilience and security;
- Resilient natural and built infrastructure;
- Strong and resilient economy; and,
- Health and wellness.
Meanwhile, CASCADESCASCADES is a multi-year capacity building initiative to address healthcare’s contribution to the climate crisis. The project is funded for a five-year term by Environment and Climate Change Canada. HealthCareCAN is a member of the CASCADES advisory committee. is creating tools to assess an organization’s readiness for sustainability and adaptation. We encourage you to check out the CASCADES playbook on organizational readiness for sustainability.
CLIMATE-RESILIENT HEALTH INFRASTRUCTURE IN CANADA
Health authorities need dependable infrastructure to withstand climate threats, achieve energy efficiency and lower GHG emissions. Because of the size of the health sector, and the fact that healthcare organizationsIncluding health authorities that operate and oversee hospitals, community care centres, primary care clinics, hospices, and long-term care facilities. across the country operate 24 hours, 7 days a week, 365 days a year, Canada’s healthcare organizations collectively account for nearly five percent of Canada’s greenhouse gas footprint[iv],[v]. Health organizations across Canada contribute to efforts to slow carbon emissions while increasing adaptability to the impacts of climate change through, for example, sustainable infrastructure and technology. Investments in green health infrastructure and the use of new technologies to reduce the health sector’s GHGs greatly enhance climate resilience. Toronto Western Hospital’s innovative use of wastewater to reduce its carbon emissions is a great example of today’s green infrastructure technology (see Box 2).
Box 2: Toronto Western Hospitals’ Green Infrastructure
Toronto Western Hospital is building the world’s largest raw wastewater energy transfer system. This system is intended to reduce the hospital’s natural gas and water usage. The new technology harnesses the thermal energy from wastewater flowing through the nearby campus sewer. The Toronto Western Hospital retrofit was funded through a Canada Infrastructure Bank investment of $19.3 million, facilitated by HealthCareCAN. It is estimated that the new wastewater energy transfer system will result in a reduction of 250,000 metric tonnes of GHGs over the next 30 years[vi].
Hospitals and healthcare organizations must be prepared to continue to provide medical care in the face of serious adverse weather events, while also operating an energy efficient, low carbon-emitting facility. Novel approaches and technologies must be adopted to not only better facilitate patient care and outcomes, but to address the impact of the health sector on the environment.[vii]
MOVING FORWARD
The World Health Organization calls climate change the greatest threat to human health in the 21st century.[viii] Healthcare organizations are already seeing the impacts of climate change arriving through their doors. During BC’s record-breaking heat wave in June 2021, 619 deaths were attributed to the extreme heat.[ix] Post-tropical storm Fiona resulted in the death of at least one person and many other injuries in Atlantic Canada recently. Already overburdened healthcare systems will face even greater pressure and must be prepared for the adverse impacts of climate change. The healthcare system must be part of the solution to limit global warming to the target of 1.5°C above pre-industrial levels.[viii]
Learn more about HealthCareCAN’s advocacy with respect to healthcare infrastructure, both physical and digital and our recommendations to government in our policy book: Strengthening the foundation of healthcare in Canada: actions to shore up healthcare and health research in Canada.
Adapting to climate change is of significant interest to members. We would like to highlight in future briefs other areas of climate change and health such as the decarbonization of the healthcare system and other low-carbon technologies. We encourage members to share with us the work your health organization is undertaking to respond to the climate challenge.
REFERENCES
[i] Berry, P., Enright, P., Varangu, L., et al. (2022). Adaptation and Health System Resilience. Health of Canadians in a Changing Climate: Advancing our Knowledge for Action. Ottawa, ON: Government of Canada.
[ii] World Health Organization. (2015). Operational framework for building climate resilient health systems. Geneva: World Health Organization.
[iii] Vancouver Coastal Health and Fraser Health. (2022). Climate change and health vulnerability and capacity assessment: summary report.
[iv] Vogel, L. (Dec. 2019) Canada’s health system is among the least green. CMAJ. 191 (48) E1342-E1343.
[v] Watts N., Amann, M., Arnell, N., et al. (2019). The 2019 report on The Lancet countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. The Lancet. 394 (10211) P1836-P1878.
[vi] Canada Infrastructure Bank. (2021). Toronto Western Hospital Retrofit. Retrieved from https://cib-bic.ca/en/projects/green-infrastructure/toronto-western-hospital-retrofit/
[vii] World Health Organization. (2020). WHO guidance for climate resilient and environmentally sustainable health care facilities. Geneva: World Health Organization.
[viii] B.C. Coroners Service. (2022). Extreme heat and human mortality: a review of heat-related deaths in B.C. in Summer 2021. Report to the Chief Coroner of British Columbia.
[ix] World Health Organization. (2021). Climate change and health. Retrieved from https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
PUBLISHED
October 21, 2022
HealthCareCAN remains attentive to the issues of our members. If your organization has any questions or feedback in connection with these or any other developments, please contact us. Your feedback is important to us, Click here to complete a survey with your suggestions for future health topics of interest.
FOR FURTHER INFORMATION
Emily Follwell
Policy and Research Analyst
efollwell@healthcarecan.dev2.inter-vision.ca
Jonathan Mitchell
Vice President – Research and Policy
jmitchell@healthcarecan.dev2.inter-vision.ca
Related:
Submission to the Federal Government’s Consultation on Artificial Intelligence (AI) Compute